Over the past few years, you may have read about the crisis in youth mental health. In October 2021, the American Academy of Pediatrics declared a national emergency in child and adolescent mental health, and in December 2021, the U.S. surgeon general highlighted the urgent need to address the nation’s youth mental health crisis. Just this month, the U.S. Preventive Services Task Force recommended screening for depression in adolescents aged 12 to 18.
October is National Depression and Mental Health Screening Month, so we’d like to highlight one of the tools WCW has been using to approach the youth mental health crisis that is in line with that recommendation: school-based mental health screenings.
Mood Check, our program, partners with schools to screen all students in designated grades and offers additional support to adolescents at high risk for depression and/or suicidal behaviors. We have a multi-pronged approach: We offer resources that increase the school community’s mental health awareness and literacy, which serves as a prevention tool. Then we provide two-level screening for students, including universal, self-reported screening for all students followed by in-depth interviews with students who are identified as high risk. We communicate with parents and guardians about youth depression and resources, and provide more significant follow-up (both immediate and long-term) for parents and guardians of high-risk teens. Finally, we offer referral access for all school families who need to find a mental health professional to help their teen moving forward.
This past school year, we screened a total of 2,078 middle and high school students in the greater Boston area for both depression and anxiety. We met one-on-one with 646 students (about 31%); 237 students (about 11%) revealed to us that they had current or past thoughts of suicide, and 57 students reported that they revealed suicidal thinking or behavior to an adult for the first time when meeting with a clinician on our team. For those who reported suicidal thinking/behavior, we introduced safety plans: a way to identify warning signs, internal coping strategies, supportive people and places, how to make the environment safe, and a motivator for living, along with providing the Suicide Prevention Lifeline phone number. Students retained a copy of the plan that they could reference themselves and/or share with parents, providers, or trusted adults.
A review of our data over time suggests that Mood Check is associated with decreased depressive symptoms in at-risk adolescents and may encourage families to seek treatment for students we identify. This kind of success in a school setting is in line with other research, which shows that teens prefer to receive mental health services in schools, rather than in mental health specialty settings. Anecdotally, we’ve found that teens are more willing to speak with us, because they know they won’t see us again; it can be easier to tell the truth to a stranger than to a parent, teacher, or guidance counselor. We’re glad to provide that listening ear for them.
School screenings alone cannot solve the crisis in youth mental health. But they are an important tool to be used in combination with depression prevention efforts and expanded access to treatment. Our goal is for more teens to be able to get the help they need in order to live healthier and happier lives.
Tracy R. G. Gladstone, Ph.D., is research director, an associate director and a senior research scientist at the Wellesley Centers for Women, where she leads the Depression Prevention Research Initiative.

 May is Mental Health Awareness Month. This year, it comes at a time when we have an increased focus on mental health due to the COVID-19 pandemic. Media reports have focused on the
May is Mental Health Awareness Month. This year, it comes at a time when we have an increased focus on mental health due to the COVID-19 pandemic. Media reports have focused on the  In 2018, I began a
In 2018, I began a  The challenges of isolation and loneliness have become apparent over the past several months of social distancing. Not only are we physically separated from our friends and extended families, but we’re concerned about their health and wellbeing as well as our own. We may be juggling childcare, homeschooling, and our own work. Or we may be wondering how we’ll support ourselves through this. We may know those who are sick, or who are high-risk, or who are essential workers putting themselves at risk for our sake. We may have lost people close to us. And we may feel powerless to do anything.
The challenges of isolation and loneliness have become apparent over the past several months of social distancing. Not only are we physically separated from our friends and extended families, but we’re concerned about their health and wellbeing as well as our own. We may be juggling childcare, homeschooling, and our own work. Or we may be wondering how we’ll support ourselves through this. We may know those who are sick, or who are high-risk, or who are essential workers putting themselves at risk for our sake. We may have lost people close to us. And we may feel powerless to do anything.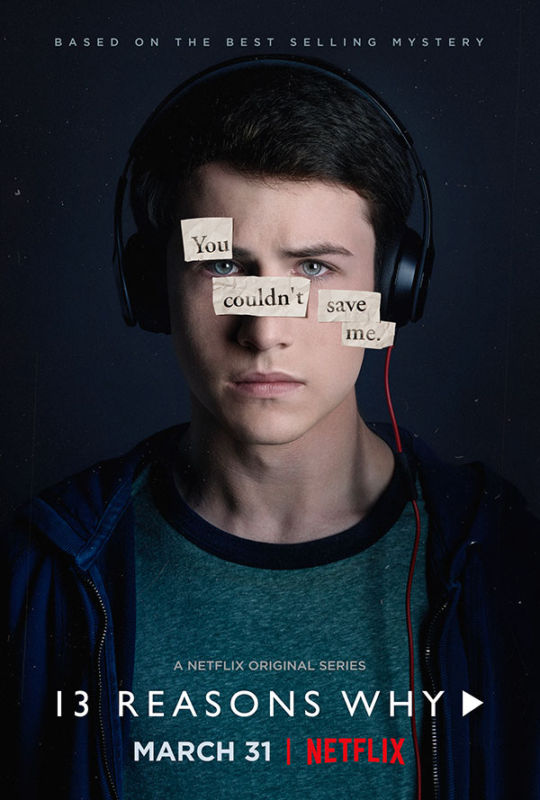
 Likewise, we worry about teens that exhibit signs of suicide. Sometimes these signs are subtle, such as giving away prized possessions, withdrawing from friends, or exhibiting significant behavioral changes, such as intense fights with family and friends. Teens thinking about suicide may also provide verbal cues, such as, “I wish I were dead” and “It’s not worth it anymore.” Also, many people who contemplate suicide do so because they believe they are a burden to others, and that they will be doing others a favor if they are no longer here. Thus, if you hear a teen say, “My family would be better off without me,” it is important to take action. Remember that 50-70 percent of people who make a suicide attempt communicate their intent prior to acting, mostly through such actions or verbal cues. Thus, if you recognize any of these signs, it is important to ASK. Although many of us find it scary to ask about suicide, or worry that asking about suicide will give someone the idea to attempt suicide, we know from numerous studies that talking about suicide will not lead to suicidal behavior.
Likewise, we worry about teens that exhibit signs of suicide. Sometimes these signs are subtle, such as giving away prized possessions, withdrawing from friends, or exhibiting significant behavioral changes, such as intense fights with family and friends. Teens thinking about suicide may also provide verbal cues, such as, “I wish I were dead” and “It’s not worth it anymore.” Also, many people who contemplate suicide do so because they believe they are a burden to others, and that they will be doing others a favor if they are no longer here. Thus, if you hear a teen say, “My family would be better off without me,” it is important to take action. Remember that 50-70 percent of people who make a suicide attempt communicate their intent prior to acting, mostly through such actions or verbal cues. Thus, if you recognize any of these signs, it is important to ASK. Although many of us find it scary to ask about suicide, or worry that asking about suicide will give someone the idea to attempt suicide, we know from numerous studies that talking about suicide will not lead to suicidal behavior. Depression is Prevalent but Prevention Programs Are Limited
Depression is Prevalent but Prevention Programs Are Limited Approaches & Recommendations
Approaches & Recommendations
 Treating youth depression once it emerges may be much more distressing, and much less effective, than identifying early symptoms of illness and treating them before they develop into a full-blown disorder. Prevention approaches have the potential to reach a large number of adolescents, and may be more acceptable than treatment because services can be rendered in non-clinical settings (e.g., schools, primary care settings), and do not require adolescents to identify themselves as ill.
Treating youth depression once it emerges may be much more distressing, and much less effective, than identifying early symptoms of illness and treating them before they develop into a full-blown disorder. Prevention approaches have the potential to reach a large number of adolescents, and may be more acceptable than treatment because services can be rendered in non-clinical settings (e.g., schools, primary care settings), and do not require adolescents to identify themselves as ill.
 So, where are all the people with mental illness? From what I hear in my office, many are hiding and suffering in silence for fear of being stigmatized, pitied, or seen as weak. American, Westernized culture plays a large role in this fear. The pervasive image of an American is a person who is strong, independent, and can
So, where are all the people with mental illness? From what I hear in my office, many are hiding and suffering in silence for fear of being stigmatized, pitied, or seen as weak. American, Westernized culture plays a large role in this fear. The pervasive image of an American is a person who is strong, independent, and can 